Understanding ‘Do Not Resuscitate’ (DNR): Debunking Popular Misconceptions
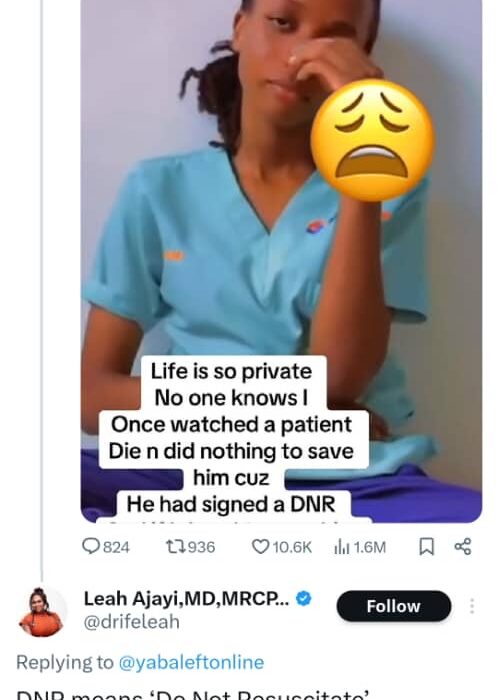
The acronym “DNR,” an abbreviation for “Do Not Resuscitate,” is often wrongly interpreted by the public, particularly when viewed on trending videos or social media commentary.
Recent conversation has brought forward common misconceptions on what specifically a DNR order is, when it would be applied, and what that would mean to patient treatment.
1. What Is a DNR?
A DNR is a medicolegal document issued by an examining medical team, not always through the patient’s or his family’s consent or decision in every case. While the reasons for issuing a DNR order are usually discussed with the patient, his or her family, or NOK, the decision lies in the hands of the clinical team based on medical rationale and ethics.
A patient can inform a doctor that they desire to be placed on a DNR, but the request must be assessed and approved by a medical professional. This includes reviewing the patient’s mental capacity and ensuring the decision is not prompted by underlying issues of mental health or suicidal intentions.
2. DNR Does Not Mean “No Treatment”
A common misunderstanding is that a DNR equates to the termination of all medical intervention. This is not true. A DNR truly translates to the fact that in the event of a cardiac or respiratory arrest, resuscitative procedures—like chest compressions, intubation, or mechanical ventilation—are not performed.
But DNR patients may and typically do receive a variety of treatments, including:
• Oxygen therapy
• Pressure support of the blood pressure in intensive care
• Dialysis
• Intravenous antibiotics and fluids
DNRs involve only withholding resuscitative care and not withholding usual or supportive care.
3. The Role of Healthcare Professionals
Healthcare professionals must counteract the tendency to view a DNR as “allowing the patient to die without doing anything.” In fact, palliative care interventions are typically instituted in DNR situations to ensure that the patient’s remaining time is spent with comfort, dignity, and compassion. Pain control and emotional support are crucial components of end-of-life treatment.
4. DNRs Are Not Permanent
It ought also to be appreciated that orders of DNRs are not for life. They can be reassessed and withdrawn based on changes in the condition, prognosis, or wish of the patient.
5. Advanced Directives
In certain situations, patients can also have “Advanced Directives” in place—legal documents that allow patients to specify their health care desires in case they are no longer capable of deciding for themselves. Such directives are useful tools for preserving patient autonomy and ensuring that medical treatment aligns with the patient’s values and preferences.
As there is greater public knowledge about end-of-life care, myths need to be dispelled and explained simply, sensitively, what DNR orders are not, and are. The health professionals and wider community must be educated about these important aspects of patient care so that patients can make informed decisions and have their care respected as dignified.